4.21 Quality Care
Ernstmeyer & Christman - Open Resources for Nursing (Open RN)
Quality is defined in a variety of ways that impact nursing practice.
ANA Definition of Quality
The American Nurses Association (ANA) defines quality as, “The degree to which nursing services for health care consumers, families, groups, communities, and populations increase the likelihood of desirable outcomes and are consistent with evolving nursing knowledge.”[1] The phrases in this definition focus on three aspects of quality: services (nursing interventions), desirable outcomes, and consistency with evolving nursing knowledge (evidence-based practice). Alignment of nursing interventions with current evidence-based practice is a key component for quality care.[2] Evidence-based practice (EBP) will be further discussed later in this chapter.
Quality of Practice is one of the ANA’s Standards of Professional Performance. ANA Standards of Professional Performance are “authoritative statements of the actions and behaviors that all registered nurses, regardless of role, population, specialty, and setting are expected to perform competently.” See the competencies for the ANA’s Quality of Practice Standard of Professional Performance in the following box.[3]
Competencies of ANA’s Quality of Practice Standard of Professional Performance[4]
- Ensures that nursing practice is safe, effective, efficient, equitable, timely, and person-centered.
- Incorporates evidence into nursing practice to improve outcomes.
- Uses creativity and innovation to enhance nursing care.
- Recommends strategies to improve nursing care quality.
- Collects data to monitor the quality of nursing practice.
- Contributes to efforts to improve health care efficiency.
- Provides critical review and evaluation of policies, procedures, and guidelines to improve the quality of health care.
- Engages in formal and informal peer review processes of the interprofessional team.
- Participates in quality improvement initiatives.
- Collaborates with the interprofessional team to implement quality improvement plans and interventions.
- Documents nursing practice in a manner that supports quality and performance improvement initiatives.
- Recognizes the value of professional and specialty certification.
Reflective Questions
- What Quality of Practice competencies have you already demonstrated during your nursing education?
- What Quality of Practice competencies are you most interested in mastering?
- What questions do you have about the ANA’s Quality of Practice competencies? Where could you find answers to those questions (e.g., instructors, preceptors, health care team members, guidelines, or core measures)?
This chapter will review content related to the competencies of the ANA’s Quality of Practice Standard of Professional Performance. Additional information about peer review is discussed in the “Leadership and Management” chapter, and specialty certification is discussed in the “Preparation for the RN Role” chapter.
Quality and Safety Education for Nurses
The Quality and Safety Education for Nurses (QSEN) project advocates for safe, quality client care by defining six competencies for prelicensure nursing students: Patient-Centered Care, Teamwork and Collaboration, Evidence-Based Practice, Quality Improvement, Safety, and Informatics. These competencies are further discussed in the “Advocacy” chapter.
Framework of Quality Health Care
A definition of quality that has historically guided the measurement of quality initiatives in health care systems is based on the framework for improvement originally created by the Institute of Medicine (IOM). The IOM name changed to the National Academy of Medicine in 2015. The IOM framework includes the following six criteria for defining quality health care[5],[6]:
- Safe: Avoiding harm to clients from the care that is intended to help them.
- Effective: Providing services based on scientific knowledge to all who could benefit and refraining from providing services to those not likely to benefit (i.e., avoiding underuse and misuse).
- Client-centered: Providing care that is respectful of and responsive to individual client preferences, needs, and values and ensuring that client values guide all clinical decisions.
- Timely: Reducing waits and sometimes harmful delays for both those who receive and those who provide care.
- Efficient: Avoiding waste, including waste of equipment, supplies, ideas, and energy.
- Equitable: Providing care that does not vary in quality because of personal characteristics such as gender, ethnicity, geographic location, and socioeconomic status.
This framework continues to guide quality improvement initiatives across America’s health care system. The evidence-based practice (EBP) movement began with the public acknowledgement of unacceptable client outcomes resulting from a gap between research findings and actual health care practices. For EBP to be successfully adopted and sustained, it must be adopted by nurses and other health care team members, system leaders, and policy makers. Regulations and recognitions are also necessary to promote the adoption of EBP. For example, the Magnet Recognition Program promotes nursing as a leader in catalyzing adoption of EBP and using it as a marker of excellence.[7]
Magnet Recognition Program
The Magnet Recognition Program is an award from the American Nurses Credentialing Center (ANCC) that recognizes organizational commitment to nursing excellence. The award recognizes organizations worldwide where nursing leaders have successfully aligned their nursing strategic goals to improve the organization’s client outcomes. To nurses, Magnet Recognition means education and development are available through every stage of their career. To clients, it means quality care is delivered by nurses who are supported to be the best that they can be.[8] See Figure 9.2[9] for an image related to the Magnet Recognition Program.

Reimbursement Models
Quality health care is also defined by value-based reimbursement models used by Medicare, Medicaid, and private insurance companies paying for health services. As discussed in the “Health Care Reimbursement Models” section of the “Health Care Economics” chapter, value-based payment reimbursement models use financial incentives to reward quality health care and positive client outcomes. For example, Medicare no longer reimburses hospitals to treat clients who acquire certain preventable conditions during their hospital stay, such as pressure injuries or urinary tract infections associated with use of catheters.[10] These reimbursement models directly impact the evidence-based care nurses provide at the bedside and the associated documentation of assessments, interventions, and nursing care plans to ensure quality performance criteria are met.
CMS Quality Initiatives
The Centers for Medicare & Medicaid Services (CMS) establishes quality initiatives that focus on several key quality measures of health care. These quality measures provide a comprehensive understanding and evaluation of the care an organization delivers, as well as clients’ responses to the care provided. These quality measures evaluate many areas of health care, including the following:[11]
- Health outcomes
- Clinical processes
- Client safety
- Efficient use of health care resources
- Care coordination
- Client engagement in their own care
- Client perceptions of their care
These measures of quality focus on providing the care the client needs when the client needs it, in an affordable, safe, effective manner. It also means engaging and involving the client, so they take ownership in managing their care at home.
Visit the CMS What is a Quality Measure web page.
Accreditation
Accreditation is a review process that determines if an agency is meeting the defined standards of quality determined by the accrediting body. The main accrediting organizations for health care are as follows:
- The Joint Commission
- National Committee for Quality Assurance
- American Medical Accreditation Program
- American Accreditation Healthcare Commission
The standards of quality vary depending on the accrediting organization, but they all share common goals to improve efficiency, equity, and delivery of high-quality care. Two terms commonly associated with accreditation that are directly related to quality nursing care are core measures and client safety goals. Please see Table 9.2 for more information on accrediting organizations.
Table 9.2. Accrediting Organizations [12], [13], [14] [15]
| Organization | Overview | History | Accreditation Process | Standards | Impact |
| The Joint Commission | Non-profit organization accrediting and certifying health care organizations and programs in the U.S. | Founded in 1951, aims to improve public health care quality and safety | Conducts rigorous on-site surveys to assess compliance with standards covering client care, medication safety, infection control, and overall performance | Developed with input from health care professionals, providers, and consumers and designed to help measure, assess, and improve performance | Recognized as a symbol of quality, reflecting commitment to high performance standards |
| National Committee for Quality Assurance (NCQA) | Private, non-profit organization improving health care quality through evidence-based standards, measures, programs, and accreditation | Established in 1990, provides quality information for health care decision-making | Comprehensive review of policies and procedures, including quality management, utilization management, credentialing, and member rights | Widely regarded standards used by CMS and state governments for quality oversight | Demonstrates commitment to improving health care quality and adhering to high performance standards |
| American Medical Accreditation Program (AMAP) | Program by AMA aimed at improving medical care quality by setting high standards for physicians | Launched in the late 1990s, assesses physicians’ qualifications and ethical standards | Detailed review process, including verification of credentials, practice history assessment, and compliance with CME requirements | Ensures physicians provide high-quality care, maintain competency, and adhere to ethical practices | Recognizes physicians’ commitment to high-quality care and medical practice standards |
| American Accreditation Healthcare Commission (AAHC) / URAC | Independent, non-profit organization promoting health care quality through accreditation, certification, and measurement | Founded in 1990, expanded from utilization review to a wide range of health care services | Thorough review of policies, procedures, and performance, including on-site visits and compliance assessment | Developed by a broad array of stakeholders to promote evidence-based practices, client safety, and continuous improvement | Recognized as a mark of excellence, demonstrating commitment to quality and accountability |
Core Measures
Core measures are national standards of care and treatment processes for common conditions. These processes are proven to reduce complications and lead to better client outcomes. Core measure compliance reports show how often a hospital successfully provides recommended treatment for certain medical conditions. In the United States, hospitals must report their compliance with core measures to The Joint Commission, CMS, and other agencies.[16]
In November 2003, The Joint Commission and CMS began work to align common core measures, so they are identical. This work resulted in the creation of one common set of measures known as the Specifications Manual for National Hospital Inpatient Quality Measures. These core measures are used by both organizations to improve the health care delivery process. Examples of core measures include guidelines regarding immunizations, tobacco treatment, substance use, hip and knee replacements, cardiac care, strokes, treatment of high blood pressure, and the use of high-risk medications in the elderly. Nurses must be aware of core measures and ensure the care they provide aligns with these recommendations.[17]
Read more about the National Hospital Inpatient Quality Measures.
National Patient Safety Goals
Patient safety goals are guidelines specific to organizations accredited by The Joint Commission that focus on health care safety problems and ways to solve them. The National Patient Safety Goals (NPSG) were first established in 2003 and are updated annually to address areas of national concern related to client safety, as well as to promote high-quality care. The NPSG provide guidance for specific health care settings, including hospitals, ambulatory clinics, behavioral health, critical access hospitals, home care, laboratory, skilled nursing care, and surgery.
The following goals are some examples of NPSG for hospitals[18]:
- Identify patients correctly
- Improve staff communication
- Use medicines safely
- Use alarms safely
- Prevent infection
- Identify patient safety risks
- Prevent mistakes in surgery
Nurses must be aware of the current NPSG for their health care setting, implement appropriate interventions, and document their assessments and interventions. Documentation in the electronic medical record is primarily used as evidence that an organization is meeting these goals.
Read the current agency-specific National Patient Safety Goals.
Next: 4.22 Measuring and Improving Quality
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- Stevens, K. R. (2013). The impact of evidence-based practice in nursing and the next big ideas. OJIN: The Online Journal of Issues in Nursing, 18(2), manuscript 4. https://ojin.nursingworld.org/MainMenuCategories/ANAMarketplace/ANAPeriodicals/OJIN/TableofContents/Vol-18-2013/No2-May-2013/Impact-of-Evidence-Based-Practice.html ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- Agency for Healthcare Research & Quality. (2022). Six domains of health care quality. https://www.ahrq.gov/talkingquality/measures/six-domains.html ↵
- Institute of Medicine (US) Committee on Quality of Health Care in America. (2001). Crossing the quality chasm: A new health system for the 21st century. National Academies Press. https://pubmed.ncbi.nlm.nih.gov/25057539/ ↵
- Stevens, K. R. (2013). The impact of evidence-based practice in nursing and the next big ideas. OJIN: The Online Journal of Issues in Nursing, 18(2), manuscript 4. https://ojin.nursingworld.org/MainMenuCategories/ANAMarketplace/ANAPeriodicals/OJIN/TableofContents/Vol-18-2013/No2-May-2013/Impact-of-Evidence-Based-Practice.html ↵
- American Nurses Credentialing Center. (2024). ANCC magnet recognition program. https://www.nursingworld.org/organizational-programs/magnet/ ↵
- “Magnet_Recognition_Logo_CMYK_-png-.png” by Mattmitchell37 is licensed under CC BY-SA 4.0 ↵
- James, J. (2012). Pay-for-performance. Health Affairs. https://www.healthaffairs.org/do/10.1377/hpb20121011.90233/full/ ↵
- CMS.gov. (2024). Quality measures. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/QualityMeasures ↵
- Joint Commission International. (2024). Who we are. https://www.jointcommission.org/?utm_campaign=tjc_brand__1_core&utm_source=google&utm_medium=cpc&gad_source=1&gclid=CjwKCAjwnK60BhA9EiwAmpHZw55yd91qdT0f3Q6nauq82Oo3uHe5nPJKBwT81CxvmdtkGrjdc26GchoCvz8QAvD_BwE ↵
- NCQA. (2024). About NCQA. https://www.ncqa.org/about-ncqa/ ↵
- AMA Ed Hub. (2024). About the AMA's CME accreditation. https://edhub.ama-assn.org/pages/ama-cme ↵
- ACHC. (2024). About accreditation. https://www.achc.org/ ↵
- John Hopkins Medicine. (n.d.). Core measures. https://www.hopkinsmedicine.org/patient_safety/core_measures.html ↵
- The Joint Commission. (n.d.). Measures. https://www.jointcommission.org/en/measurement/measures/ ↵
- The Joint Commission. (2025). 2025 national patient safety goals. https://www.jointcommission.org/standards/national-patient-safety-goals/ ↵
Advocacy
The American Nurses Association (ANA) emphasizes that advocacy is fundamental to nursing practice in every setting. See Figure 10.1[1] for an illustration of advocacy. Advocacy is defined as the act or process of pleading for, supporting, or recommending a cause or course of action. Advocacy may be for individuals, groups, organizations, communities, society, or policy issues[2]:
- Individual: The nurse educates health care consumers so they can consider actions, interventions, or choices related to their own personal beliefs, attitudes, and knowledge to achieve the desired outcome. In this way, the health care consumer learns self-management and decision-making.[3]
- Interpersonal: The nurse empowers health care consumers by providing emotional support, assistance in obtaining resources, and necessary help through interactions with families and significant others in their social support network.[4]
- Organization and Community: The nurse supports cultural and social transformation of organizations, communities, or populations. Registered nurses understand their obligation to help improve environmental and societal conditions related to health, wellness, and care of the health care consumer.[5]
- Policy: The nurse promotes inclusion of the health care consumers’ voices into policy, legislation, and regulation about issues such as health care access, reduction of health care costs and financial burden, protection of the health care consumer, and environmental health, such as safe housing and clear water.[6]
Advocacy at each of these levels will be further discussed in later sections of this chapter.
Advocacy is one of the ANA’s Standards of Professional Performance. The Standards of Professional Performance are “authoritative statements of the actions and behaviors that all registered nurses, regardless of role, population, specialty, and setting, are expected to perform competently."[7] See the following box to read the competencies associated with the ANA’s Advocacy Standard of Professional Performance.[8]
Competencies of ANA’s Advocacy Standard of Professional Performance[9]
- Champions the voice of the health care consumer.
- Recommends appropriate levels of care, timely and appropriate transitions, and allocation of resources to optimize outcomes.
- Promotes safe care of health care consumers, safe work environments, and sufficient resources.
- Participates in health care initiatives on behalf of the health care consumer and the system(s) where nursing happens.
- Demonstrates a willingness to address persistent, pervasive systemic issues.
- Informs the political arena about the role of nurses and the vital components necessary for nurses and nursing to provide optimal care delivery.
- Empowers all members of the health care team to include the health care consumer in care decisions, including limitation of treatment and end-of-life care.
- Embraces diversity, equity, inclusivity, health promotion, and health care for individuals of diverse geographic, cultural, ethnic, racial, gender, and spiritual backgrounds across the life span.
- Develops policies that improve care delivery and access for underserved and vulnerable populations.
- Promotes policies, regulations, and legislation at the local, state, and national levels to improve health care access and delivery of health care.
- Considers societal, political, economic, and cultural factors to address social determinants of health.
- Role models advocacy behavior.
- Addresses the urgent need for a diverse and inclusive workforce as a strategy to improve outcomes related to the social determinants of health and inequities in the health care system.
- Advances policies, programs, and practices within the health care environment that maintain, sustain, and restore the environment and natural world.
- Contributes to professional organizations.
Reflective Questions
- What Advocacy competencies have you already demonstrated during your nursing education?
- What Advocacy competencies are you most interested in performing next?
- What questions do you have about ANA’s Advocacy competencies?
Next: 2.12 Individual and Interpersonal Advocacy
Nurses advocate for issues in their communities and their organizations.
Addressing Social Determinants of Health
Advocacy is commonly perceived as acting on behalf of a client, but it can be a much broader action than affecting a single client and their family members. Nurses advocate for building healthier communities by addressing social determinants of health (SDOH). SDOH are the conditions in the environments where people live, learn, work, and play that affect a wide range of outcomes. SDOH include health care access and quality, neighborhood and environment, social and community context, economic stability, and education access and quality. Social determinants of health (SDOH) have a major impact on people’s health, well-being, and quality of life. See Figure 10.2[10] for an illustration of SDOH.[11]

Specific examples of addressing SDOH include the following goals:
- Improving safe housing and public transportation
- Decreasing discrimination and violence
- Expanding quality education and job opportunities
- Increasing access to nutritious foods and physical activity opportunities
- Promoting clean air and clean water
- Enhancing language and literacy skills[12]
SDOH contribute to health disparities and inequities among different socioeconomic groups. For example, individuals who don't have access to grocery stores with healthy foods are less likely to have good nutrition, increasing their risk for health conditions like heart disease, diabetes, and obesity, and potentially lowering their life expectancy relative to people who do have access to healthy foods.[13]
One of Healthy People 2030’s goals specifically relates to advocacy regarding SDOH. The goal states, “Create social, physical, and economic environments that promote attaining the full potential for health and well-being for all.” Across the United States, people and organizations at the local, state, territorial, tribal, and national levels are working hard to improve health and reduce health disparities by addressing SDOH.[14] Read more information about these advocacy efforts in the following box.
Read more about efforts addressing SDOH at Healthy People 2030.
Understanding and addressing SDOH is crucial for effective health care advocacy, as it provides a comprehensive view of the various elements that impact clients' well-being. These determinants include economic stability, education, social and community context, health and health care access, and the neighborhood and built environment.
Organization Advocacy
Nurses advocate for organizational issues in the nursing profession and the workplace through participation in unions, collective bargaining, workplace advocacy models, and professional organizations.
Unions and Collective Bargaining
A nursing union is a type of labor union that advocates for the interest of its nurse members. According to the Bureau of Labor Statistics, 20 percent of RNs and 10 percent of LPNs/VNs in the United States are union members.[16] Nursing union goals are typically to advocate for the improvement of benefits, wages, client safety, and workplace conditions. Advocacy is accomplished by collective bargaining. Collective bargaining refers to the negotiation of wages and other conditions of employment by an organized body of employees. See Figure 10.3[17] for an image of a union worker.

Although there is no single union that represents all nurses across the country, there are several nursing unions such as the National Nurses United, SEIU United Healthcare, and The United Food and Commercial Workers International Union. The National Nurses United union is the largest nursing union in the United States and has joined with other unions across the country to address unsafe staffing. Read more about these unions in the following box.
Read more about nursing unions:
Nursing unions can provide several potential benefits to the nursing profession. They may improve job security, improve working conditions, negotiate for better pay and benefits, protect seniority, establish staffing ratios, address workplace violence and incivility, and provide a well-defined grievance process. Unionized nurses earn an average of $200-$400 more per week than nonunionized nurses. Unions assist with grievance processes for resolving disagreements between employees and management. Examples of grievances include the promotion of one employee over another who has more seniority, disputes over holiday pay, and problems related to employee discipline.[18]
However, there are also potential disadvantages of unions, such as the cost of dues (up to $90/month per nurse), difficulty in removal of incompetent nurses, mandatory strikes with no pay, the issue of seniority taking precedence over good performance, and creation of working environments that can be adversarial between management and nursing. Additionally, many nursing unions are not organized or led by nurses, causing the belief that some unions are more interested in collecting dues than in improving the work environment for nurses. Although there has been research to determine if unions are good for nurses and good for clients, the findings are not conclusive. Some studies have shown that unionized hospitals have lower mortality rates, but higher failure-to-rescue and pressure injury rates. Another study found that unionized hospitals had higher levels of job dissatisfaction but higher levels of nurse retention.[19],[20]
Workplace Advocacy Models
Nurses can advocate for improvements in the workplace via various mechanisms, such as shared governance and the ANCC Magnet Recognition Program, and by participation in professional organizations. Nurses can also seek legislative solutions for workplace problems by advocating for legislation such as whistleblower protection.[21] Whistleblower protection is further discussed in the "Policy Advocacy" section of this chapter.
Shared Governance
Shared governance refers to a shared leadership model between management and employees working together to achieve common goals. Shared governance models are believed to promote nurses’ empowerment, engagement, autonomy, accountability, and collaboration while also striving to improve client safety, quality care, and positive outcomes. This style of management encourages and empowers nurses to be part of making decisions that impact their daily work environments. When organizations utilize a shared governance model, employees feel valued and invested in the organization's success. Nurse engagement also improves both staff and client outcomes, such as increased job satisfaction and client satisfaction.[22] Implementation of a shared governance model has led to organizational cost savings, decrease in meeting times, fewer sick days used by employees, and a decrease in staff turnover.[23] See the following box for an example of effective shared governance.
Example of Effective Shared Governance[24]
A busy telemetry unit wants to address issues with low client satisfaction scores and an increase in both central line and indwelling catheter days. A quality improvement project is instituted by a multidisciplinary team that works to communicate the project's goals and objectives, respecting each team member's expertise and input. The team initiates daily multidisciplinary rounding on the unit. Six months after the implementation of multidisciplinary rounding, client satisfaction scores improve, and a decrease in both central line and indwelling catheter days is noted. Multidisciplinary rounding provides a collaborative team approach, acknowledging the expertise and leadership role of each discipline with the same end goal of improving client outcomes.
Magnet Recognition Program
Nurses can advocate for their excellence in the workplace by participating in activities required for Magnet Recognition. As previously discussed in this book, the Magnet Recognition Program is an organizational credential from the American Nurses Credentialing Center (ANCC) recognizing quality client outcomes, nursing excellence, and innovations in professional nursing practice. The Magnet Recognition Program requires nursing advocacy in the areas of technology, education, policies, and process development. This advocacy is accomplished by creating unit-based practice councils who meet regularly to discuss unit policies, practices, and outcomes. Additionally, an organization-wide practice council includes a representative from each unit council and reviews organizational-wide policies and practices. Read more about the Magnet Recognition Program in the following box.
Read more about the Magnet Recognition Program.
Professional Nursing Organizations
Professional organizations provide easy access to nursing advocacy work being done across the nation and the world. There are over 100 local, state, and national organizations that advocate for the nursing profession. Professional nursing organizations may advocate for specific nursing issues in certain areas of practice, such as critical-care nursing (American Association of Critical-Care Nurses, AACN) or broader national nursing issues, such as the American Nurses Association (ANA). Professional organizations also provide opportunities for continuing education, advanced certification, and participation in political action committees. Membership in state and national organizations helps nurses stay up-to-date on current evidence-based practices and research findings.
Next: 2.14 Policy Advocacy
National, state, and local policies impact nurses at all levels of care, from nurse administrators to bedside nurses, making it essential for nurses to take an active role in advocating for their clients, their profession, and their community. Nurses advocate for improved access to basic health care, enhanced funding of health care services, and safe practice environments by participating in policy discussions. Nurses also participate in state and national policy discussions affecting nursing practice. For example, nurses advocate for the removal of practice barriers so nurses can practice according to the full extent of their education, certification, and licensure; address reimbursement based on the value of nursing care; and expand funding for nursing education.[25]
When advocating, nurses must view themselves as knowledgeable professionals who have the power to influence policy and decision-makers. A nurse can advocate for improved policies through a variety of pathways. Each method provides a unique opportunity for the nurse to impact the health of individuals and communities, the profession of nursing, and the overall health care provided to clients. These are few easy ways for nurses to get involved:
- Becoming involved in professional nursing organizations
- Engaging in conversations with local, state, and federal policymakers on health care related issues
- Participating in shared governance committees regarding workplace policies
Health Care Legislative Policies
Legislative policies are external rules and regulations that impact health care practice and policy at the national, state, and local levels. These regulations seek to protect clients and nurses by defining safe practices, quality standards, and requirements for health care organizations and insurance companies. Nurses have been involved in the adoption of these rules and regulations and continue to advocate for new and updated legislation affecting health care.
Examples of federal legislation addressing health care include advocating for the Patient’s Bill of Rights, client privacy and confidentiality, improved access to health care, and protections for individuals who report unethical or illegal activities in the health care environment (i.e., whistleblower legislation). Examples of legislation at the state level includes topics such as right-to-die and physician-assisted suicide, medicinal marijuana use, and nurse-to-client staffing ratios.
Review how client rights are defined by policies at the federal, state, and organizational levels in the following box.
Client’s Rights Defined at Multiple Levels
In 1973 the American Hospital Association (AHA) adopted the Patient’s Bill of Rights. The bill has since been updated and adapted for use throughout the world in all health care settings, but, in general, it safeguards a client’s right to accurate and complete information, fair treatment, and self-determination when making health care decisions. In 2010 the Affordable Care Act was passed at the federal level. It included additional client rights and protections for health care consumers in the areas of preexisting conditions, choice of providers, and limited lifetime coverage limits imposed by insurance companies.
States further define client rights beyond federal regulations and provide specific rights of health care consumers in their state. For example, Wisconsin’s Department of Health Services defines treatment rights, protections for records privacy and access, communication rights, personal rights, and privacy rights.
Read more about Patient Rights in the American Healthcare System.
Visit the CMS web page to read more about the Affordable Care Act and the revised Patient’s Bill of Rights.
Research advocacy policies in your state. Here is Wisconsin’s law regarding client rights.
Nurses’ Roles in Legislative Policies
With over four million registered nurses in the United States, nursing has a powerful voice that can significantly influence health care legislation. Nurses have been recognized as a major influence on health care policies related to client safety and quality care. They can become involved in policy making at the state and federal level by joining a professional nursing organization, communicating with their state representatives, or running for political office to take an active role in policy creation.
Most professional nursing organizations have a legislative policy committee that reviews proposed federal and state legislation and makes recommendations for change, endorses the legislation, or leads opposition. For example, organizations such as the American Nurses Association (ANA), National League of Nursing (NLN), and state nursing associations inform members of current legislative initiatives, provide comprehensive reviews, and encourage members to contact their representatives about pending legislation.
Read more about current advocacy efforts by the Wisconsin Nurses Association.
Whistleblowing
Nurses are expected to follow federal, state, and agency policies and regulations, be proactive in policy development, and speak up when policies are not being followed. When regulations and policies are not being followed, nurses must advocate for public safety by reporting the problem to a higher authority. Whistleblowing refers to reporting a significant concern to your supervisor, the federal or state agency responsible for the regulation, or in the case of criminal activity, to law enforcement agencies. A whistleblower is a person who exposes any kind of information or activity that is deemed illegal, unethical, or not correct within an organization. See Figure 10.5[26] for federal instructions regarding whistleblowing.
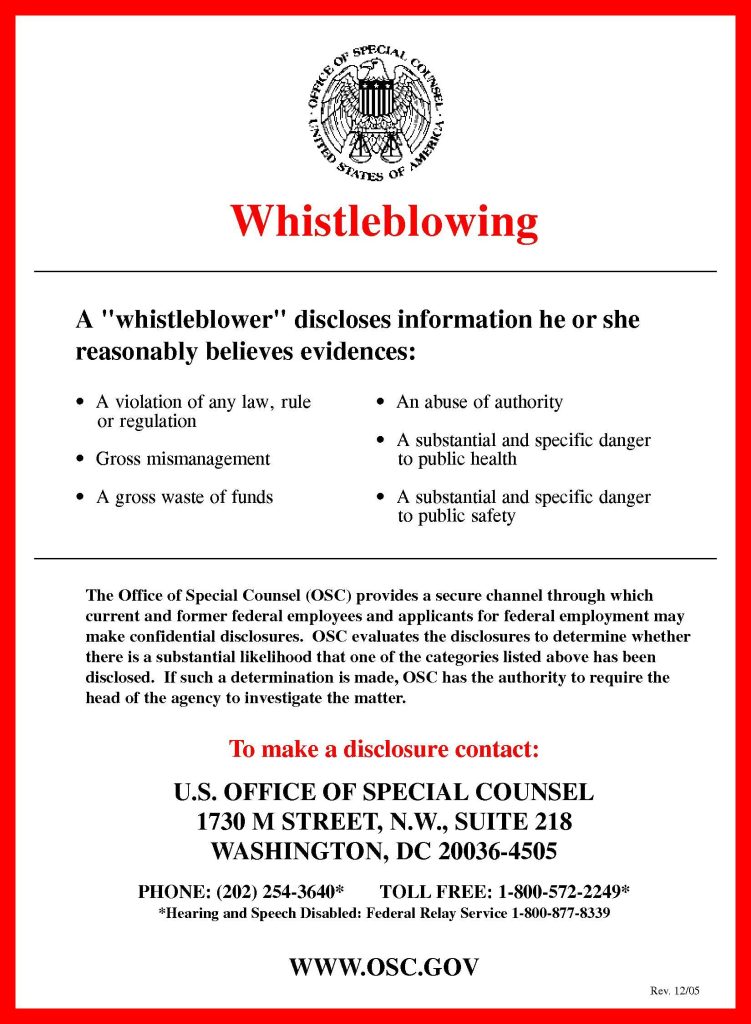
Whistleblowing typically begins with reporting the wrongdoing to a supervisor and following the internal chain of command. This first step of reporting allows the organization to correct the issue internally. However, there may be situations where an individual may need to directly report to an external authority, such as a State Board of Nursing or another regulatory agency. For example, any person who has knowledge of conduct by a licensed nurse violating state or federal law may report the alleged violation to the State Board of Nursing where the conduct occurred.
Acting as a whistleblower can be a difficult decision because the individual may be labelled “disloyal” or potentially face retaliatory actions by the accused individual or organization. Although there are legal protections for whistleblowers, these types of actions may occur. Read important information from the ANA regarding whistleblowing in the following box.
ANA Information Regarding Whistleblowing[27]
- If you identify an illegal or unethical practice, reserve judgment until you have adequate documentation to establish wrongdoing.
- Do not expect those who are engaged in unethical or illegal conduct to welcome your questions or concerns about this practice.
- Seek the counsel of someone you trust outside of the situation to provide you with an objective perspective.
- Consult with your state nurses’ association or legal counsel if possible before taking action to determine how best to document your concerns.
- Remember, you are not protected in a whistleblower situation from retaliation by your employer until you blow the whistle.
- Blowing the whistle means that you report your concern to the national and/or state agency responsible for regulation of the organization for which you work or, in the case of criminal activity, to law enforcement agencies as well.
- Private groups, such as The Joint Commission or the National Committee for Quality Assurance, do not confer protection. You must report to a state or national regulator.
- Although it is not required by every regulatory agency, it is a good rule of thumb to put your complaint in writing.
- Document all interactions related to the whistleblowing situation and keep copies for your personal file.
- Keep documentation and interactions objective.
- Remain calm and do not lose your temper, even if those who learn of your actions attempt to provoke you.
- Remember that blowing the whistle is a very serious matter. Do not blow the whistle frivolously. Make sure you have the facts straight before taking action.
Next: 2.15 Steps to Becoming an Advocate
To become a nursing advocate, identify causes, issues, or needs where YOU can exert influence.
Steps to becoming an advocate include the following[28]:
- Identify a problem that interests you: Start by pinpointing a specific issue or area within nursing that you are passionate about. This could range from client safety and quality of care to workplace conditions and professional development opportunities.
- Research the subject and select an evidence-based intervention: Conduct thorough research on the identified issue. Look for evidence-based practices and interventions that have been proven to address or mitigate the problem effectively. Gathering robust data will help you build a solid case for your advocacy efforts.
- Network with experts who are, or could be, involved in making the change: Connect with professionals and experts who are either already involved in addressing the issue or who could play a crucial role in implementing changes. Building a network of like-minded individuals can provide support, resources, and additional perspectives.
- Work hard for change: Advocacy requires dedication and persistence. Actively participate in efforts to bring about the desired change. This might include engaging in public speaking, writing articles or blogs, meeting with policymakers, or organizing community events to raise awareness.
Once you have identified a topic of interest, it's crucial to get involved in activities that can amplify your advocacy efforts:
- Committees: Volunteer to participate in committees that review and develop practice policies within your health care institution.
- Professional Nursing Organizations: Become a member of state and national nursing organizations. These groups often provide valuable resources, including access to current legislative and policy initiatives, public policy agendas, and ways to get involved.
- Research and Review: Stay informed by researching best practices and reviewing the health policy agendas of elected officials. Understanding the current landscape will help you identify opportunities to influence policy and practice.
Nurses hold a powerful position to be effective advocates due to their frontline role in health care delivery. Their unique insights into client care, the work environment, and health care systems make them valuable voices in policy discussions. As the largest sector of the health care workforce, nurses have significant potential to influence decisions at every level.
Advocating for change can lead to improved quality of care, better client outcomes, and safe work environments. By pushing for evidence-based practices and policies, nurses can help ensure that clients receive the best possible care. Advocacy efforts focused on client safety and quality can directly impact client health and recovery. Additionally, nurses can advocate for better working conditions, which can lead to a safer and more supportive environment for all healthcare workers.
Imagine the impact if every nurse actively engaged in advocacy. The collective efforts could drive substantial improvements in health care delivery and policy, leading to positive changes across the profession.
Review information about a new professional nursing association called the Nurse Advocacy Association.